Mucormycosis is a fungal infection that affects the sinuses and lungs after inhaling fungal spores in the air. This infection has a low frequency in the past, with cases documented mostly in people with uncontrolled diabetes. However, numerous hospitals across the India recently are reporting an elevation in infections of COVID‑19‑associated mucormycosis (CAM).
SO, let’s know more about that!!
What is mucormycosis?
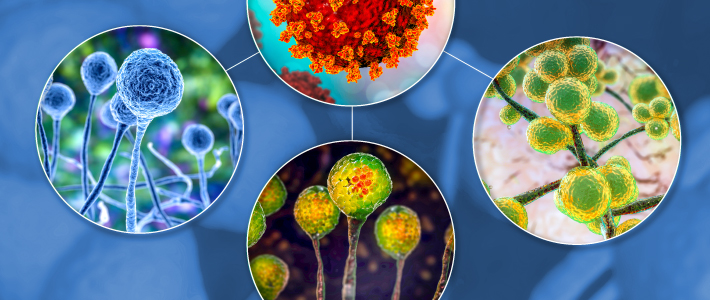
- Mucormycosis (sometimes called zygomycosis) is a serious but rare fungal infection caused by a group of molds called mucoromycetes. These fungi live throughout the environment. They live in soil and in decaying organic matter, such as leaves, compost piles, or rotten wood.
- People get mucormycosis by coming in contact with the fungal spores in the environment. For example, infections involving the lung or sinus can occur after someone breathes in spores. These forms of mucormycosis usually occur in people who have health problems or take medicines that lower the body’s ability to fight germs and sickness.

Symptoms of Mucormycosis:
The symptoms of mucormycosis depend on where in the body the fungus is growing.
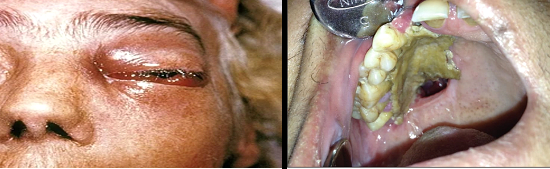
- Symptoms of rhinocerebral (sinus and brain) mucormycosis include:
- One-sided facial swelling
- Headache
- Nasal or sinus congestion
- Black lesions on nasal bridge or upper inside of mouth that quickly become more severe
- Fever
- Symptoms of pulmonary (lung) mucormycosis include:
- Fever
- Cough
- Chest pain
- Shortness of breath
- Cutaneous (skin) mucormycosis can look like blisters or ulcers, and the infected area may turn black. Other symptoms include pain, warmth, excessive redness, or swelling around a wound.

- Symptoms of gastrointestinal mucormycosis include:
- Abdominal pain
- Nausea and vomiting
- Gastrointestinal bleeding
- Disseminated mucormycosis typically occurs in people who are already sick from other medical conditions, so it can be difficult to know which symptoms are related to mucormycosis. Patients with disseminated infection in the brain can develop mental status changes or coma.
How does someone get mucormycosis?
People get mucormycosis through contact with fungal spores in the environment. For example, the lung or sinus forms of the infection can occur after someone inhales the spores from the air. A skin infection can occur after the fungus enters the skin through a scrape, burn, or other types of skin injury.
Is mucormycosis contagious?
No. Mucormycosis can’t spread between people or between people and animals.
Deaths due to it
- Mucormycosis is frequently a life-threatening infection. A review of published mucormycosis cases found an overall all-cause mortality rate of 54%. The mortality rate varied depending on underlying patient condition, type of fungus, and body site affected (for example, the mortality rate was 46% among people with sinus infections, 76% for pulmonary infections, and 96% for disseminated mucormycosis).
- Mucormycosis is an uncommon, invasive, and fungal opportunistic infection that can be life threatening. It is caused by contact with mucor mold, which can be found in soil, air, and even human noses and mucus. It erodes facial structures as it progresses through the respiratory tract.
- Patients die within days of contracting the disease, and in other cases, doctors have had to remove eyes and upper jaws to prevent the life‑threatening infection from spreading.

Risks factors associated with Mucormycosis in COVID‑19
Mucormycosis is more common in coronavirus patients who have a weaker immune system and diabetes. Mucormycosis, which is uncommon in India, has emerged as a new problem for COVID‑19 patients on steroid therapy and those with diabetes. Strong steroids used to treat severe COVID‑19 can reduce immunity and increase sugar levels, thereby helping the spread of “black fungus” and increasing its frequency. Along with a large number of COVID‑19 patients, India has millions who suffer from diabetes, which might also raise the risk of a black fungus infection. Many treatments used to treat COVID‑19 decrease the body’s immune system, which would typically defend the individual from a fungal infection.
- Corticosteroid therapy
- Diabetes
- organ transplant
- persistent neutropenia
- skin trauma, burns, or surgical wounds
- iron overload
- malnourishment
are all risk factors for mucormycosis
How is mucormycosis diagnosed?
Healthcare providers consider your medical history, symptoms, physical examinations, and laboratory tests when diagnosing mucormycosis. Healthcare providers who suspect that you have mucormycosis in your lungs or sinuses might collect a sample of fluid from your respiratory system to send to a laboratory. Your healthcare provider may perform a tissue biopsy, in which a small sample of affected tissue is analyzed in a laboratory for evidence of mucormycosis under a microscope or in a fungal culture. You may also need imaging tests such as a CT scan of your lungs, sinuses, or other parts of your body, depending on the location of the suspected infection.

How is it treated?
Mucormycosis is a serious infection and needs to be treated with prescription antifungal medicine, usually amphotericin B, posaconazole, or isavuconazole. These medicines are given through a vein (amphotericin B, posaconazole, isavuconazole) or by mouth (Posaconazole, isavuconazole). Other medicines, including fluconazole, voriconazole, and echinocandins, do not work against fungi that cause mucormycosis. Often, It requires surgery to cut away the infected tissue.
Prevention of Fungal Infections in Patients with Covid‑19
- Mucormycosis is difficult to prevent because it is transferred by inhaling mold spores in soil, rotting vegetables or bread, or compost piles. It is usually not passed from person to person, but it is found in the environment. The possibility of aspergillosis must be considered in patients with severe COVID‑19 who have abnormal respiratory function, even if they do not have apparent risk factors for aspergillosis. In patients with severe COVID‑19 fungal co‑infections, early detection, and surveillance for Candida and antifungal resistance diseases (e.g., C. auris, azole‑resistant Aspergillus) are critical to minimizing death from COVID‑19
- It is one of serious opportunistic infections and economic cost that can associated with COVID‑19 infection. Much is stay unclear about the consequences of SARS‑CoV‑2 virus and its correlations with other diseases.
- The use of steroid drugs for treating COVID‑19 may partially explain the surge in these fungal infections, along with weakened immune systems from COVID‑19; corticosteroids impair migration, ingestion, and engulfment activity in human macrophages. Hyperglycemia and acidosis have been shown to inhibit phagocytic cell chemotaxis and killing activity against Mucorales by weakening both oxidative and nonoxidative mechanisms.
- it has a high mortality rate and can be seen in other parts of the worlds is possible because Mucorales are found in environment so it may be found in any part in spite of they are not contiguous from person to another. Physicians have to prescribe the right dose of cortisone. We should ensure that people who have diabetes should keep monitoring their sugar levels. As well as, we have to wear two masks, because it can be found in air, especially places like construction sites
- https://www.cdc.gov/
- Al-Khikani FH. Mucormycosis “Black Fungus” new challenge associated with COVID 19. Biomed Biotechnol Res J 2021;5:267-71
- https://blogs.medibuddy.in/
