Polycystic Ovary Syndrome (PCOS) is the most common endocrinologic condition in women, affecting between 8-13% of reproductive aged women. It is an enigmatic condition that while extremely common, creates challenges in the diagnosis and management, as leading symptoms may vary based on age, and treatment may be tailored to specific requirements of individual need
Signs and symptoms of PCOS often develop around the time of the first menstrual period during puberty. Sometimes PCOS develops later, for example, in response to substantial weight gain.
Signs and symptoms of PCOS vary. A diagnosis of PCOS is made when you experience at least two of these signs:
- Irregular periods. Infrequent, irregular or prolonged menstrual cycles are the most common sign of PCOS. For example, you might have fewer than nine periods a year, more than 35 days between periods and abnormally heavy periods.
- Excess androgen. Elevated levels of male hormones may result in physical signs, such as excess facial and body hair (hirsutism), and occasionally severe acne and male-pattern baldness.
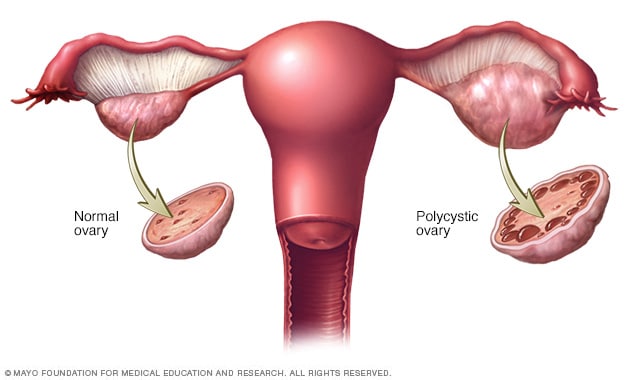
- Polycystic ovaries. Your ovaries might be enlarged and contain follicles that surround the eggs. As a result, the ovaries might fail to function regularly.

- We must first mention a quick word about the hormonal mechanism of the normal menstrual cycle. It is known that the cycle begins with the gonadotropin-releasing hormone (GnRH) secreted from the hypothalamus, prompting the pituitary to secrete both luteinizing hormone (LH) and follicle-stimulating hormone (FSH). At the beginning of the follicular phase, luteinizing hormone stimulates the theca cells in the ovary to secrete androgenic hormones, and at the same time, follicle-stimulating hormone stimulates granulosa cells to convert androgenic hormones into estrogen (principally estradiol), which is important in the development and growth of the follicle. During this phase, the levels of estradiol increase significantly, which leads to an increase in the concentration of LH and the occurrence of the so-called “jump” of this hormone. In the middle of the cycle and thus the maturation of the follicle and the occurrence of ovulation.

- By the time the diagnosis is established, PCOS presents as a phenotype reflecting a selfperpetuating vicious cycle involving neuroendocrine, metabolic, and ovarian dysfunction
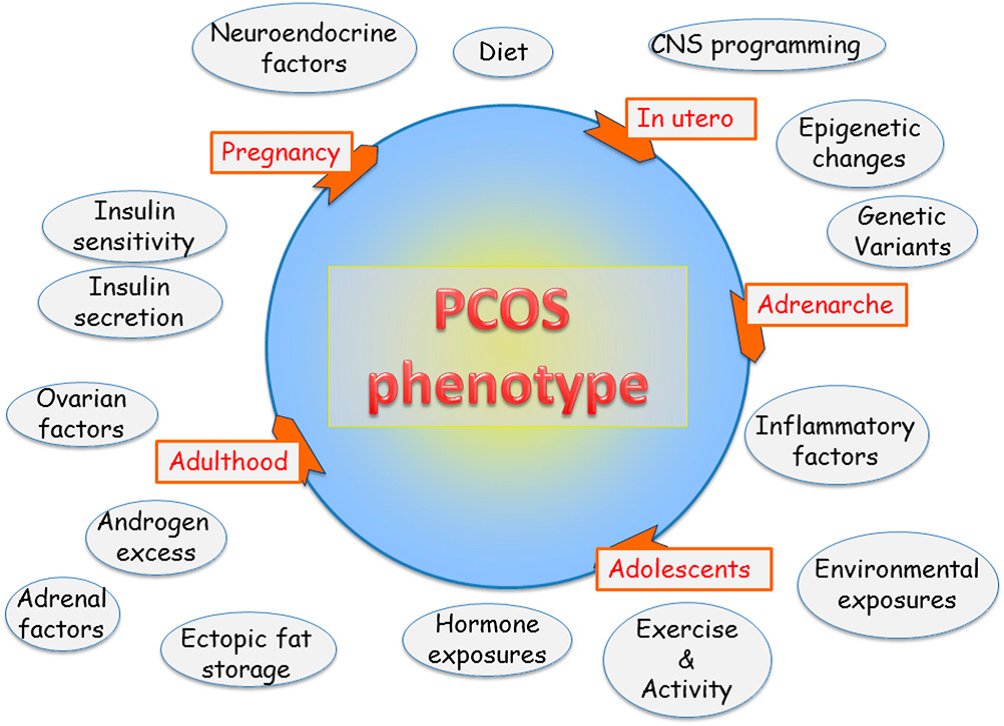
- The pathogenesis of polycystic ovary syndrome (PCOS) is not precisely known. There are several mechanisms that have been suggested to play a role in the pathogenesis of PCOS, including hormonal imbalance, insulin resistance, and genetic inheritance.
- Hormonal Involvement : PCOS is associated with abnormal production and metabolism of hormones, such as androgens and estrogen, in the body. There are typically high levels of androgenic hormones such as testosterone, androstenedione, and dehydroepiandrosterone sulfate (DHEA-S), although there is often considerable variation among patients.
Some research has suggested that :
- the secretion of luteinizing hormone (LH) from the anterior pituitary gland increases the stimulatory effect on the ovarian theca cells and may lead to the raised levels of androgenic hormones and irregular or absent ovulation.
- The level of follicle stimulating hormone (FSH) is reduced with respect to LH, which reduces the reaction to aromatize the androgen hormones to estrogen. As a result, there is less estrogen available and ovulation may not be able to occur.
- also linked the CYP450 C17 enzyme to PCOS as the rate-limiting step for the synthesis of androgenic hormones such as testosterone in the body. Although further research is needed to support this, abnormalities in this enzyme or the presence of other substances that inhibit or induce this enzyme may be involved in the pathogenesis of PCOS.
2- Insulin Resistance :
There is a strong correlation between PCOS and resistance to insulin the body. This may be secondary to an abnormality in the binding to the insulin receptors, resulting in changes in the signaling pathways. It has been suggested that the raised levels of insulin alter the effect of gonadotropins and the function of the ovaries, leading to PCOS.
Specifically, the excess insulin may cause the ovaries to produce more testosterone and alter the development of follicles needed for ovulation to take place. Ovulation may be inhibited or delayed as a result, leading to PCOS.
The effect of insulin resistance in the pathogenesis of PCOS is amplified when a woman is overweight or obese. The excess fat can worsen the resistance to insulin and, therefore, lead to more severe symptoms associated with the condition.
Another hormone called adiponectin that is involved in the control of lipid and glucose levels in the blood might also play a role in the pathogenesis of the condition. Higher concentrations of this hormone are usually evident in women affected by PCOS.
3- Genetic Inheritance :
Research investigating a genetic link to the pathogenesis of PCOS has suggested an autosomal dominant pattern of inheritance in families with a history of the condition. Fathers may be carriers of the genetic abnormality and may display some characteristics of PCOS, such as excessive hair growth.
Some studies have investigated the role of regulatory genes of the CYP17, CYP19, FST, and INSR enzymes in association with PCOS. Of these, there may be susceptibility in the INSR gene, although the research is not sufficient to claim that in may cause the condition. Other studies have investigated other genes, such as PON1 and IGF2. However, it remains unclear which specific gene mutation may cause PCOS in women.
Complications of PCOS can include:
- Infertility
- Gestational diabetes or pregnancy-induced high blood pressure
- Miscarriage or premature birth
- Metabolic syndrome — a cluster of conditions including high blood pressure, high blood sugar, and abnormal cholesterol or triglyceride levels that significantly increase your risk of cardiovascular disease
- Type 2 diabetes or prediabetes
- Sleep apnea
- Depression, anxiety and eating disorders
- Abnormal uterine bleeding
- Cancer of the uterine lining (endometrial cancer)
Obesity is associated with PCOS and can worsen complications of the disorder.
The PCOS Consensus Workshop Group has proposed a review of diagnostic criteria, defining PCOS as the presence of at least two of the following criteria together:
- Oligo-anovulation
- Hyperandrogenism with clinical or biochemical signs
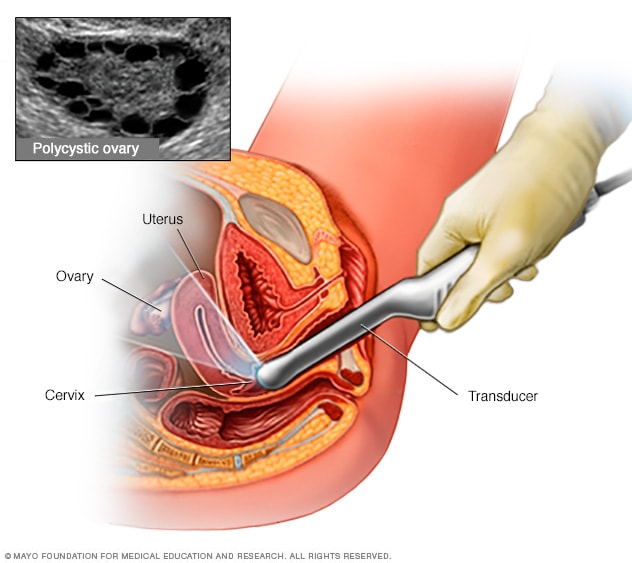
- Polycystic ovary appearance on ultrasound examination
In order to establish the diagnosis of PCOS, it is important to exclude other disorders with a similar clinical presentation, such as congenital adrenal hyperplasia, Cushing’s syndrome, and androgen-secreting tumors.
Are any tests needed?
Tests may be advised to clarify the diagnosis and to rule out other hormone conditions.
- Blood tests may be taken to measure certain chemicals (hormones). For example, a test to measure the male hormone testosterone and luteinising hormone (LH) which tend to be high in women with PCOS.
- An ultrasound scan of the ovaries may be advised. An ultrasound scan is a painless test that uses sound waves to create images of structures in the body. The scan can detect the typical appearance of PCOS with the many small cysts (follicles) in slightly enlarged ovaries
- Also, you may be advised to have an annual screening test for diabetes or impaired glucose tolerance (pre-diabetes). A regular check for other cardiovascular risk factors such as blood pressure and blood cholesterol, may be advised to detect any abnormalities as early as possible. Exactly when and how often the checks are done depends on your age, your weight and other factors. After the age of 40, these tests are usually recommended every three years.
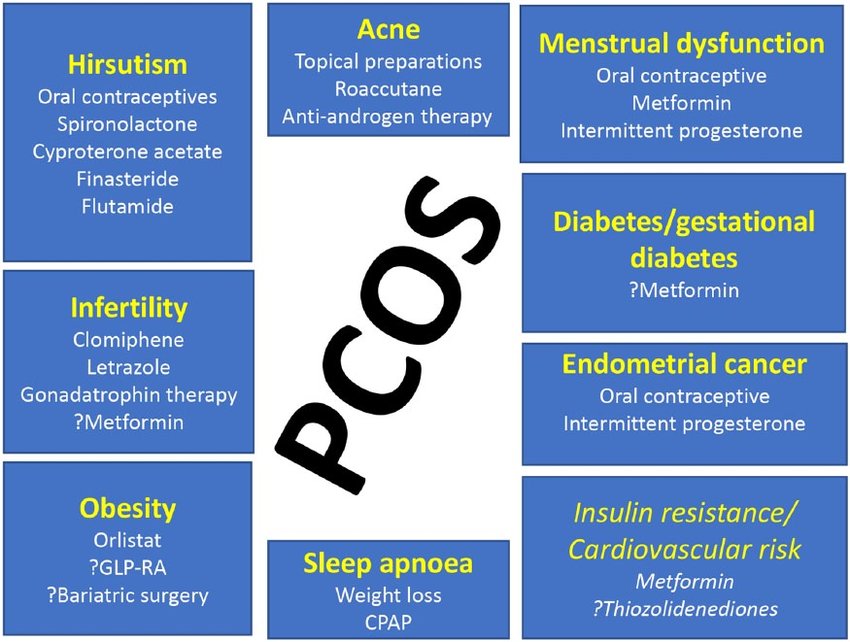
PCOS treatment focuses on managing your individual concerns, such as infertility, hirsutism, acne or obesity. Specific treatment might involve lifestyle changes or medication.
Medications
To regulate your menstrual cycle, your doctor might recommend:
- Combination birth control pills. Pills that contain estrogen and progestin decrease androgen production and regulate estrogen. Regulating your hormones can lower your risk of endometrial cancer and correct abnormal bleeding, excess hair growth and acne. Instead of pills, you might use a skin patch or vaginal ring that contains a combination of estrogen and progestin.
- Progestin therapy. Taking progestin for 10 to 14 days every one to two months can regulate your periods and protect against endometrial cancer. Progestin therapy doesn’t improve androgen levels and won’t prevent pregnancy. The progestin-only minipill or progestin-containing intrauterine device is a better choice if you also wish to avoid pregnancy.
To help you ovulate, your doctor might recommend:
- Clomiphene. This oral anti-estrogen medication is taken during the first part of your menstrual cycle.
- Letrozole (Femara). This breast cancer treatment can work to stimulate the ovaries.
- Metformin. This oral medication for type 2 diabetes improves insulin resistance and lowers insulin levels. If you don’t become pregnant using clomiphene, your doctor might recommend adding metformin. If you have prediabetes, metformin can also slow the progression to type 2 diabetes and help with weight loss.
- Gonadotropins. These hormone medications are given by injection.
To reduce excessive hair growth, your doctor might recommend:
- Birth control pills. These pills decrease androgen production that can cause excessive hair growth.
- Spironolactone (Aldactone). This medication blocks the effects of androgen on the skin. Spironolactone can cause birth defects, so effective contraception is required while taking this medication. It isn’t recommended if you’re pregnant or planning to become pregnant.
Lifestyle and home remedies:
To help decrease the effects of PCOS, try to:
- Maintain a healthy weight. Weight loss can reduce insulin and androgen levels and may restore ovulation. Ask your doctor about a weight-control program, and meet regularly with a dietitian for help in reaching weight-loss goals.
- Limit carbohydrates. Low-fat, high-carbohydrate diets might increase insulin levels. Ask your doctor about a low-carbohydrate diet if you have PCOS. Choose complex carbohydrates, which raise your blood sugar levels more slowly.
- Be active. Exercise helps lower blood sugar levels. If you have PCOS, increasing your daily activity and participating in a regular exercise program may treat or even prevent insulin resistance and help you keep your weight under control and avoid developing diabetes.
summary
- Hoeger, K. M., Dokras, A., & Piltonen, T. (2021). Update on PCOS: consequences, challenges, and guiding treatment. The Journal of Clinical Endocrinology & Metabolism, 106(3), e1071-e1083.
- Rotterdam ESHRE/ASRM‐Sponsored PCOS Consensus Workshop Group. (2004). Revised 2003 consensus on diagnostic criteria and long‐term health risks related to polycystic ovary syndrome (PCOS). Human reproduction, 19(1), 41-47.
- Witchel, S. F., Oberfield, S. E., & Peña, A. S. (2019). Polycystic ovary syndrome: pathophysiology, presentation, and treatment with emphasis on adolescent girls. Journal of the Endocrine Society, 3(8), 1545-1573
- http://www.nhs.uk/Conditions/Polycystic-ovarian-syndrome/Pages/Causes.aspx
- http://www.mayoclinic.org/diseases-conditions/pcos/basics/causes/con-20028841
- https://medlineplus.gov/ency/article/000369.htm
- http://patient.info/health/polycystic-ovary-syndrome-leaflet
- http://emedicine.medscape.com/article/256806-overview#a4
